The Sleeve Gastrectomy
 The sleeve gastrectomy has gained tremendous popularity over the last 5 years. This is the result of several short-term studies documenting excellent weight loss results, akin to the gastric bypass. The acceptably low risk of serious complications has also been demonstrated. Based off these findings many insurance carriers have begun to cover this procedure.
The sleeve gastrectomy has gained tremendous popularity over the last 5 years. This is the result of several short-term studies documenting excellent weight loss results, akin to the gastric bypass. The acceptably low risk of serious complications has also been demonstrated. Based off these findings many insurance carriers have begun to cover this procedure.
What is not well known amongst the patient population is that the sleeve gastrectomy has been around for 25 years. The sleeve gastrectomy is a key component of the biliopancreatic diversion procedure, a procedure uncommonly performed today. In some patients of extreme BMI the biliopancreatic diversion was performed in two stages. The first stage was to perform the sleeve gastrectomy allowing the patient to lose sufficient weight before proceeding with the second, more risky part. What many surgeons noted was that sleeve patients were enjoying excellent weight loss and improvement in several medical conditions caused or exacerbated by weight. These findings led the bariatric surgical community to examine the sleeve gastrectomy as a “stand alone” procedure. The findings have been convincing.
Restriction
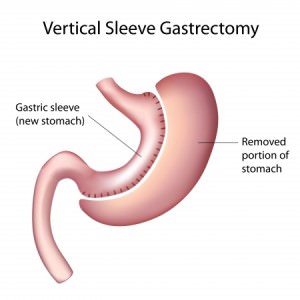
The laparoscopic sleeve gastrectomy is a procedure that involves removing the majority of the stomach. Approximately 75-80% of the stomach is removed. The resected segment of stomach comprises, the greater curvature, the portion of the stomach that has tremendous ability to distend and accommodate large volumes of food. The patient maintains direct continuity between esophagus, stomach and small intestine. This procedure is purely restrictive. There are no bypassed segments of small intestine.
The shape of the stomach is similar to a banana. Patients will find that they are full or satisfied after significantly smaller meals.
Weight Loss
The laparoscopic sleeve gastrectomy appears to have a similar weight loss profile to the gastric bypass. In the first 6 months many patients will obtain 30-40% excess weight loss. At one year the amount of excess weight loss in between 50-60%. Between 18 months and 2 years patients generally have achieved between 60-80% excess weight loss.
An appropriate diet, dedicated exercise and an active lifestyle are paramount to maintaining weight. Reverting to old habits has a high probability of causing weight regain.
Complications in Sleeve Gastrectomy
All surgery poses the risk of having a complication. Patients are at risk for complications that aren’t unique to bariatric surgery. Fortunately, the majority of complications that occur are generally not life threatening and can be managed without further surgery. Complications after laparoscopic sleeve gastrectomy are categorized as “early” and “late” complications. Early complications are generally those that occur right around the time of surgery or within the first 30 days. Late complications generally occur from one month to years after the procedure.
Early complications
Bleeding
Significant blood loss or hemorrhage is an uncommon event. The source of blood loss is usually from the dense network of blood vessels that surround the stomach. The spleen shares a common circulation with the greater curvature of the stomach. These vessels must be divided to remove the large portion of stomach. Injury to the spleen can be a source of significant blood loss and even a need for complete removal of the spleen to obtain control. Another source of bleeding that can occur after the surgery has been completed is from the staple lines that are necessary to divide the stomach. Staple line bleeding is usually “self-limited”, meaning it will likely stop on its own. Although the need for blood transfusion is uncommon it may be necessary as a life saving maneuver.
Staple-line leak
The most dreaded complication is a staple-line “leak”. A leak can be devastating if not managed quickly and appropriately. A leak can lead to peritonitis, a potentially deadly form of intra-abdominal infection. The risk of having a leak has been estimated to be around 1.0%.
Deep Vein Thrombosis/Pulmonary Embolism
DVT (deep vein thrombosis) is when a blood clot forms within the veins of the pelvis or leg. A DVT can cause leg swelling and pain. A DVT can be life threatening if the clot dislodges and travels to the heart and is then pumped into the pulmonary (lung) arteries. This is referred to as a PE (pulmonary embolism). A PE can place significant strain on the heart and if left untreated can have major consequences. Treatment requires the use of a blood thinner for a period of 3 months to a full year. In some cases, medical treatment with a blood thinner could be life-long.
Several precautions are taken to reduce the chances of developing a DVT/PE. This includes the use of blood thinners prior to and after surgery. In some patients blood thinners may be necessary even after discharge. In addition, SCD (serial compression device) boots are placed on the patients lower legs prior to surgery and remain in place until the patient is up into a chair and walking.
The risk of developing a DVT depends on a number of factors. Dr Laker will be able to give you an idea of what your risk is based on your history and a number of other factors. Overall, the risk of developing a DVT is quite small, approximately 0.5-2%. Of those patients who develop a DVT the risk of having a PE is also very low.
Wound infection
Infections at the incision sites are uncommon when the procedure is performed in a laparoscopic fashion. However, should your operation need to be converted to an open procedure there is substantially higher risk for developing a surgical site infection. Post-operative wound infections can generally be treated with local wound care (dressing changes) and sometimes a course of antibiotics.
Death
Large studies have demonstrated that potentially of dying as a result of complications after gastric bypass surgery are very low and around 0.25%.
Late complications
Persistent reflux and difficulty swallowing
The size of the sleeve can have major implications in the postoperative period. Sleeves that are too narrow can lead to or aggravate existing reflux. In addition, a sleeve that is too narrow can also make it difficult for food to enter the stomach and pass through. The area of narrowing can sometimes be dilated using endoscopy. This essentially “stretches” the area and allows food to more readily pass across the area. In some patients repeated endoscopies may be necessary until the sleeve has been appropriately dilated.
Vitamin/mineral deficiencies
Dietary indiscretions and failure to take vitamins and mineral supplements can be the source of vitamin and mineral deficiencies. This is generally well managed by taking the vitamin and mineral supplements as recommended by Dr Laker. Blood work should be obtained twice annually for the first year or two after surgery and then annually.
Gallstone formation
Rapid weight loss can predispose patients to develop gallstones. Should the gallstones become symptomatic patients may require gallbladder surgery.
Hernia
Hernias at the incision sites are uncommon when the procedure is performed laparoscopically. However, should your operation need to be converted to an open procedure there is a substantially higher risk for developing a hernia. Wound infections also increase the chances of developing a hernia as do obesity and diabetes.
Regaining Weight
Approximately two years after surgery some patients will regain 5-10% of the total weight initially lost. In time, the sleeve dilates and can accommodate larger volumes of food. An appropriate diet, dedicated exercise and an active lifestyle are paramount to maintaining weight. Reverting to old habits has a high probability of causing weight regain.
