Anatomy and General Function
 The colon, also known as the large intestine, is a hollow organ of approximately 5 feet in length. Although much shorter in length than the small intestine, the term “large intestine” refers to its much larger diameter.
The colon, also known as the large intestine, is a hollow organ of approximately 5 feet in length. Although much shorter in length than the small intestine, the term “large intestine” refers to its much larger diameter.
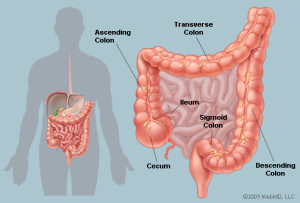
The colon is divided into anatomical segments based off blood supply and adjacent organs. The first portion of the colon is the cecum. The appendix projects off the cecum and within inches is the junction between the small intestine and colon. This is referred to as the ileocecal junction. The colon generally forms an inverted “U” as it ascends the right side of the abdomen (ascending colon), crosses the abdomen from right to left (transverse colon) and descends down the left abdomen(descending colon) to the “S” shaped sigmoid colon. The sigmoid colon empties into the rectum. Although the rectum is a continuation of the sigmoid colon there are a host of anatomic, mechanical and functional differences. Diseases of the colon and rectum are often managed in a different fashion.
The function of the colon, in general, is the recycling of fluid, electrolytes and unabsorbed nutrients. The small intestine is generally responsible for the absorption of ingested nutrients (protein, fat, carbohydrates, vitamins and minerals). Digestion and absorption requires several liters of fluid rich enzymes to enter the GI tract. A large volume of fluid along with some electrolytes and nutrients pass from the small intestine into the colon. The colon absorbs approximately 90% of the fluid and electrolytes that pass through preventing continuous diarrhea and major fluid losses.
The colon has more than 400 different bacterial species that play a key role in maintaining colon integrity, immune function and overall health. It is estimated that every gram of stool contains approximately 100 billion-1 trillion bacteria! The natural colonic bacteria (flora) breakdown indigestible fiber providing a nutrient by-product that is the preferred energy source for the cells lining the inside of the colon. In addition, bacteria are involved in the absorption of important vitamins such as Vitamin K.
When is colon surgery needed?
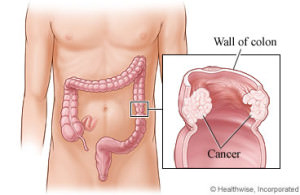 There are a number of diseases that may require surgical intervention. One of the more common reasons for colon surgery is for colon cancer. Colon cancer screening generally begins at the age of 50 with the use of colonoscopy. Colonoscopy is a procedure where a long slender tube with a camera is placed into the rectum and allows examination of the inner lining of the entire colon. Individuals with a family history of colon cancer usually will have their first colonoscopy prior to age 50. Colonoscopy can identify growths within the colon. These growths are called polyps. The majority of polyps are benign, however, there is strong evidence that some cancers will arise from certain polyps. Colonoscopy also allows for biopsy and sometimes complete removal of the polyp.
There are a number of diseases that may require surgical intervention. One of the more common reasons for colon surgery is for colon cancer. Colon cancer screening generally begins at the age of 50 with the use of colonoscopy. Colonoscopy is a procedure where a long slender tube with a camera is placed into the rectum and allows examination of the inner lining of the entire colon. Individuals with a family history of colon cancer usually will have their first colonoscopy prior to age 50. Colonoscopy can identify growths within the colon. These growths are called polyps. The majority of polyps are benign, however, there is strong evidence that some cancers will arise from certain polyps. Colonoscopy also allows for biopsy and sometimes complete removal of the polyp.
Indications for colon surgery are: biopsy proven colon cancer, inability to remove an entire polyp or the polyp is located in an area that excision may lead to other complications. 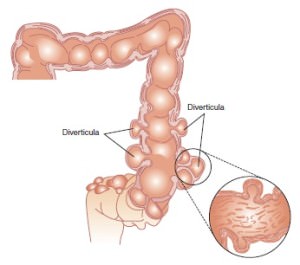
The most common indication for colon surgery for benign disease is diverticulosis. Diverticulum are small out-pouchings of the wall of the colon. Colonic diverticulum are common and it is estimated that 30 % of people older than 50 have diverticulum. About 60% of individuals over 85 have diverticulum. The majority of diverticulum are seen in the sigmoid and descending colon, however, some individuals may develop diverticulum in the cecum, ascending colon and throughout the entire colon.
Colonic diverticulum have a propensity to bleed or become inflamed and can be a source of colon perforation. Recurrent episodes of bleeding requiring blood transfusions is a strong indicator for surgery. Perforation from an inflamed diverticulum (diverticulitis) can be a surgical emergency. Sometimes small contained perforations can be managed with bowel rest and IV antibiotics. Recurrent episodes of inflammation (diverticulitis) is another indicator for surgery.
Laparoscopic Colon Surgery
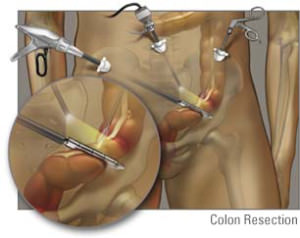 At one time, laparoscopic colon surgery was limited to benign disease such as diverticulitis. The concern with laparoscopic surgery for colon cancer stemmed from the idea that the ability to harvest lymph nodes in the resected specimen was not as good when performed in an open fashion. There have been several studies that have shown the ability to harvest lymph nodes to be equivalent when performed by a surgeon skilled in laparoscopic techniques. Laparoscopic surgery can now safely be performed for malignant diseases of the colon with equivalent oncologic results.
At one time, laparoscopic colon surgery was limited to benign disease such as diverticulitis. The concern with laparoscopic surgery for colon cancer stemmed from the idea that the ability to harvest lymph nodes in the resected specimen was not as good when performed in an open fashion. There have been several studies that have shown the ability to harvest lymph nodes to be equivalent when performed by a surgeon skilled in laparoscopic techniques. Laparoscopic surgery can now safely be performed for malignant diseases of the colon with equivalent oncologic results.
The benefits of laparoscopic surgery in colon cancer are:
- Reduced wound complications (infection and hernia)
- Shorter hospital stay
- Decreased pain
- Earlier return to work/activity
In some cases laparoscopic surgery may not be possible or the surgeon may convert to an open approach during the procedure. Previous abdominal surgeries, scar tissue, tumor size and degree of inflammation are major determining factors.
