Hernias of the Groin - Inguinal Hernia
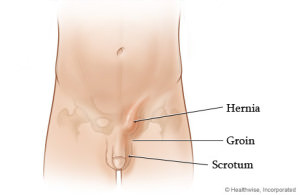
The groin is the lowest part of the abdominal wall. The area spans from the top of the iliac crest (hip bone) across the abdomen and extends down to the pubic bone and the junction of the thigh and lower abdomen.
Inguinal Hernia
 Most inguinal hernias occur in men and a small percentage of women develop inguinal hernias. The reason for the much higher prevalence in men relates to major anatomical and embryologic differences.
Most inguinal hernias occur in men and a small percentage of women develop inguinal hernias. The reason for the much higher prevalence in men relates to major anatomical and embryologic differences.
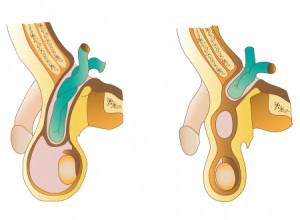
In the male fetus, the testicle develops in the abdominal cavity and descends over time to it’s final location within the scrotum. The layers of the abdominal wall descend along with the testicle and become other structures surrounding testicle. The inner most lining is in communication with the abdominal cavity. Normally, this inner lining disappears and the connection between the abdominal cavity and scrotum is obliterated. In 5% of men this communication persists and intra-abdominal contents can slide into the inguinal canal and scrotum. This is referred to as an indirect inguinal hernia and is considered congenital. In other words, it’s a groin hernia that a person is born with.
When women develop inguinal hernias it is almost always of the indirect variety. The mechanism of formation is different but the end result is the same lining sliding alongside a uterine ligament that traverses the inguinal canal and anchors into the pubic bone.
Another factor that contributes to a higher prevalence in males is due to major differences in boney pelvis anatomy between sexes. The inguinal floor in males is generally broader and subjected to internal forces at higher pressures. This promotes gradual weakening of the floor and eventual eventration or bowing outward of the muscular floor. This type of hernia has been referred to as a direct inguinal hernia. This type of inguinal hernia is thought to develop as the result of “wear and tear”.
How are hernias repaired?
Inguinal hernias can be repaired in an open or laparoscopic fashion both with and without mesh. Mesh free repairs are referred to as primary repairs and several techniques have been described over the last century. In the past 30 years the use of mesh has become increasingly used. At this time most surgeons will use mesh as it has been demonstrated to reduce the incidence of hernia recurrence. In the last 20 years there has been increasing use of laparoscopic techniques to repair groin hernias. Laparoscopic techniques almost always require mesh for satisfactory repair.
What is the difference between open and laparoscopic techniques?
The open repair requires a 4-6 inch oblique incision in the groin. The hernia(s) are identified and reduced (pushed back into place). Mesh is typically placed on top of the inguinal floor increasing its strength and durability and covering the potential openings through which tissue can slide. This is referred to as an “onlay” technique.
The laparoscopic techniques allow complete visualization of the inguinal region including the femoral space. Once the anatomy is delineated and the hernia(s) are reduced, mesh is placed under the abdominal wall defects. This is referred to as an “underlay”.
What are the advantages of the laparoscopic and robotic techniques?
When inguinal hernias are approached from within the abdominal cavity or just outside the abdominal cavity (preperitoneal) the entire inguinal floor can be visualized. The entire area of weakness can be reinforced or covered. The open technique only exposes a small area of the inguinal floor and thus wide coverage is difficult to obtain.
Laparoscopic and robotic inguinal hernia repair enables repair of the left and right sides simultaneously through three small incisions. Minimally invasive repair has also been demonstrated to be beneficial in those patients who are undergoing surgery for recurrent inguinal hernias. The recovery is generally quicker and with less pain and swelling. Patients are generally able to return to work sooner and most patients can return to full activity within 3 to 4 weeks.
What is the recurrence rate for repaired inguinal hernias?
When performed by highly trained and experienced surgeons that recurrence rate is identical between open and laparoscopic hernias and is 1-2%.
Types of Inguinal Hernias
The groin is the lowest part of the abdominal wall. The area spans from the top of the iliac crest (hip bone) across the abdomen and extends down to the pubic bone and the junction of the thigh and lower abdomen.
The majority of inguinal hernias happen to men and a much smaller percentage of women develop inguinal hernias. The incidence appears to favor men to women in the range of 20:1. The reason for the higher incidence among men relates to anatomical and developmental differences between the two genders. Some literature reports a man’s lifetime risk of developing am inguinal hernia may be as high as 20%. No wonder hernias have been depicting in the human story since the beginning of time. Inguinal hernias are classified as either inborn or acquired.
Inguinal Hernia: inborn
During embryologic development the teste develops within the abdominal cavity. The arterial supply of the testicles comes directly from the aorta (the largest artery in the body) the lies deep inside the abdominal cavity. The blood returns from the testicle to the heart through a series of veins that either drain directly into the vena cava (the largest vein in the body) or to the left kidney vein.
During the final stages of fetal development the teste begins its descent from inside the abdominal cavity through an opening of the lower abdominal wall and eventually into the scrotum. The layers of muscle and connective tissue of the abdominal wall descend with the testicle and become other structures. The deepest layer is continuous with the peritoneum, a bag that surrounds the organs of the abdominal cavity. This extension of the lining is called the processus vaginalis and is expected to disappear, obliterating the opening between the abdominal cavity and scrotum. In 5-7% of males the processus vaginalis remains and intra-abdominal contents can slide into the inguinal canal and scrotum. This has historically been referred to as an “indirect” inguinal hernia. These hernias are considered congenital, something that an individual is born with. Women can also develop inguinal hernias of the indirect variety. The round ligament, an anchoring ligament of the uterus, moves through a much smaller opening of the abdominal wall and anchors directly to the pubic bone. A hernia sac can slide alongside the ligament allowing for herniation. Because the inguinal tunnel is larger in men physical exam allows for passage of a finger into the canal and hernias can be appreciated. This is the classic “turn and cough” part of the physical exam. The same examination cannot be performed in women because the canal is much too small. This is why making the diagnosis of inguinal hernias can be so difficult in women if a visible bulge is not present. Ultrasound can often be used to help establish the diagnosis.
Inguinal hernia: acquired
The abdominal wall consists of three layers of muscle, each surrounded by a layer of connective tissue called fascia both on top of and below the muscles. The fascia converges in the midline to cover the rectus muscles along the anterior abdominal wall. This muscular and fascial arrangement changes in the lower abdominal wall. In order for the blood supply to the testes to move through the abdominal wall the muscles begin to form a series of archways. This leads to a relatively “bare area” of the lower abdominal wall. The area of greatest weakness is the floor of the inguinal canal. The floor consists of a thin layer of connective tissue. In other words, the dense muscle and strong fibrous connective tissue found throughout the abdominal wall is virtually non-existent in the groin. The inguinal floor in males is generally broader and subjected to internal forces at higher pressures.
Men are commonly employed in jobs that requires repetitive forceful movements and heavy lifting subjecting the lower abdomen to exceptionally high stresses. This promotes gradual weakening of the floor and eventual eventration or bowing outward of the muscular floor. This type of hernia has been referred to as a direct inguinal hernia. This type of inguinal hernia is thought to develop as the result of “wear and tear”. Men also tend to store excess fat within the abdominal cavity and this too increases intra-abdominal pressure.