Epigastric Hernia
What is an epigastric hernia?
An epigastric hernia is a defect of the abdominal wall in the midline between the breastbone and umbilicus (belly button). Often, patients experience a pinching or pulling sensation with exertion or certain movements. At times there may be a visible bulge in the area of pain. The pinched tissue is usually fat that lies just above the inner lining of the abdominal cavity. The majority of these hernias can be repaired using sutures alone.
How is an Epigastric Hernia Fixed?
The type of repair for an epigastric hernia is related to the size of the abdominal wall defect. The larger the defect the more likely it is to recur after repair with only sutures. A repair that uses only sutures to close an opening in the abdominal wall is referred to as a “primary repair”. The surgical literature has demonstrated a higher likelihood of hernia recurrence when umbilical hernias more than 2 cm (0.75 inches) are repaired primarily. Therefore, most surgeons utilize mesh when performing an umbilical hernia repair for a defect larger than 2 cm.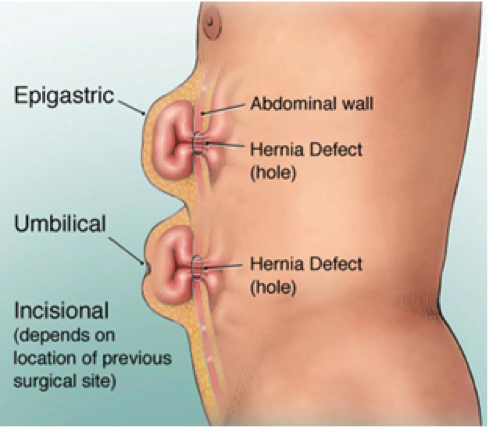
Can an epigastric hernia be repaired with minimally invasive surgery?
Epigastric hernias can be repaired laparoscopic and robotic fashion and it is the method that I prefer. The most common reason for a recurrence is failure to provide enough coverage of the defect with mesh. Using laparoscopic and robotic techniques, mesh is placed underneath the defect, in surgery this is referred to as an “underlay”. Laparoscopic repair allows for excellent vision of the defect and provides a method for securing an appropriate sized mesh around the defect and in a secure manner.
A recently described technique to address ventral hernias (umbilical, epigastric, Spigelian and incisional) is called eTEP (expanded totally extra-peritoneal) and this can be performed both robotically as well as laparoscopic. The eTEP takes advantage of the layered architecture of the abdominal wall. The mesh is placed in between layers of the abdominal wall, thereby, acting as an underlay patch and in direct contact with musculature. The abdominal cavity is not entered and therefore there is no contact between the mesh and the underlying abdominal organs. At the same time, the mesh is in an ideal location for full tissue integration and incorporation. This diminishes the potential for infections, chronic pain and likely recurrence.
Dr Laker has performed many eTEPs both robotically and laparoscopically to correct hernias of the abdominal wall.
